The Injury Rehabilitation Problem:

-
Over $600B is spent annually in the USA due to musculoskeletal (MSK) injuries.[i]
-
With most injuries, thousands of sensory receptors are destroyed, resulting in chronic joint instability.[ii] [iii] [iv]
-
Most injury rehab patients have trouble not only with activating and coordinating their muscles but also with processing sensory information.[v]
-
In injury rehab, high-level motor unit activation refers to the ability to engage and control specific groups of muscle fibers effectively. This involves the precise and efficient use of muscles, requiring strong neural connections and coordination. Injuries can disrupt these connections, leading to challenges in muscle control, strength and renewed performance and a much higher prevalence of subsequent injuries.[vi]
-
Overuse injuries often result in muscle imbalances in the body, which affect performance.[vii]
-
Progressive physical therapy rehabilitation tools are necessary to advance muscle adaptation and control following an injury or surgery, and ALL muscle layers must be fired for strength and stability recovery, but no progressive training systems like this are available without being prohibitively expensive.
-
Patient physical therapy compliance and continuation at home are major factors in enhancing post injury recovery.[viii]
Balance-Strength™ Training Can Improve & Accelerate Injury Rehabilitation:
-
Numerous scientific studies show dynamic balance training for proprioception is an essential component in recovery from an injury or surgery by restoring dynamic stability and fine motor control at an injured joint for a more functional return to everyday activities & sports.[ix] [x] [xi]
-
Dynamic balance training also facilitates body awareness with the benefit of “remembered” reactions to imbalance created in training situations. Balance awareness becomes an innate, automatic skill. The ideal balance program for injury rehab is one that challenges both static and dynamic balance with a focus on coordination.[xii]
-
Athletes and everyday people rehab from injuries faster when an effective Balance-Strength™ training system is employed. [xiii]
-
If injured structures of the brain, nerves, and muscles are never challenged, they will never be forced to heal, adapt, and improve (neuroplasticity, myoplasticity) in their functional capabilities. [xiv] [xv] [xvi]
-
Improvements in neuro-muscular functional capabilities can translate to a reduction in recurrence of MSK injuries.[xvii]
ZeSa’s Dynamic Balance-Strength Training System™ Enhances Injury Rehab: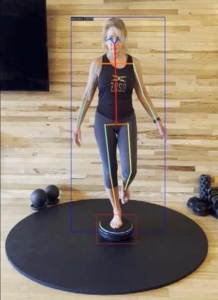
-
The peripheral nervous system can regenerate, and ZeSa’s system provides the interaction needed to help accomplish nerve regeneration and muscle recovery through neural pathway stimulation, safely and effectively.[xviii]
-
Progressive tools are necessary to increase muscle healing and control when treating injury, and ALL muscle layers must be firing for strength and stability growth (known as Dynamic Stability). [xix] The ZeSa system provides these tools and is fully progressive over a large capability range.
-
ZeSa’s system provides non-impact training methods, which are important for injury rehabilitation to challenge the anatomy but not cause additional degradation.[xx] [xxi]
-
ZeSa’s Dynamic Balance-Strength Training System™ trains the neuromuscular system and stabilizes and strengthens the entire MSK system after injury, including ligaments and tendons that surround joints most prone to overuse and injury (i.e., ankles, knees, hips, and shoulders). This mitigates joint instability and re-injury while simultaneously training major skeletal muscles and the associated stabilizing muscles.[xxii]
-
The ZeSa system is perfect for home-use therapy after injury or surgery to supplement physical therapy sessions, speed up recovery, and continue long-term health benefits.[xxiii]
-
Use of the ZeSa system is fun and simple and can be an excellent method to encourage physical therapy program compliance between office visits and after physical therapy programs are completed for continued long-term injury recovery.[xxiv]
[i] https://www.hingehealth.com/resources/press-releases/2022-state-of-msk-report/
[ii] Hertel J. Functional Anatomy, Pathomechanics, and Pathophysiology of Lateral Ankle Instability. J AthlTrain. 2002 Dec;37(4):364-375. PMID: 12937557; PMCID: PMC164367.
[iii] TayfurB, CharuphongsaC, Morrissey D, Miller SC. Neuromuscular Function of the Knee Joint Following Knee Injuries: Does It Ever Get Back to Normal?ASystematic Review with Meta-Analyses. Sports Med. 2021 Feb;51(2):321-338. doi: 10.1007/s40279-020-01386-6. PMID: 33247378; PMCID: PMC7846527.
[iv] Chatzilamprinos K, Semaltianou E, Hatzimanouil D, Lytras D, Sykaras E. Evaluation of Strength and Functional Ability of Soccer Players Two Years After Anterior Cruciate Ligament Reconstruction: A Cross-sectional Study. J Musculoskelet Neuronal Interact. 2024 Mar 1;24(1):55-66. PMID: 38427369; PMCID: PMC10910195.
[v] Asan AS, McIntosh JR, Carmel JB. Targeting Sensory and Motor Integration for Recovery of Movement After CNS Injury. Front Neurosci. 2022 Jan 21;15:791824. doi: 10.3389/fnins.2021.791824. PMID: 35126040; PMCID: PMC8813971.
[vi] Gokeler A, Neuhaus D, Benjaminse A, Grooms DR, Baumeister J. Principles of Motor Learning to Support Neuroplasticity After ACL Injury: Implications for Optimizing Performance and Reducing Risk of Second ACL Injury. Sports Med. 2019 Jun;49(6):853-865. doi: 10.1007/s40279-019-01058-0. Erratum in: Sports Med. 2019 Jun;49(6):979. doi: 10.1007/s40279-019-01078-w. PMID: 30719683; PMCID: PMC6548061.
[vii] Neme JR. Balancing Act: Muscle Imbalance Effects on Musculoskeletal Injuries. Mo Med. 2022 May-Jun;119(3):225-228. PMID: 36035582; PMCID: PMC9324710.
[viii] Kattan AE, AlHemsi HB, AlKhawashki AM, AlFadel FB, Almoosa SM, Mokhtar AM 2nd, Alasmari BA. Patient Compliance With Physical Therapy Following Orthopedic Surgery and Its Outcomes. Cureus. 2023 Apr 6;15(4):e37217. doi: 10.7759/cureus.37217. PMID: 37159781; PMCID: PMC10163936.
[ix] Winter L, Huang Q, Sertic JVL, Konczak J. The Effectiveness of Proprioceptive Training for Improving Motor Performance and Motor Dysfunction: A Systematic Review. Front Rehabil Sci. 2022 Apr 8;3:830166. doi: 10.3389/fresc.2022.830166. PMID: 36188962; PMCID: PMC9397687.
[x] Alahmari, K.A., Kakaraparthi, V.N., Reddy, R.S. et al. Combined Effects of Strengthening and Proprioceptive Training on Stability, Balance, and Proprioception Among Subjects with Chronic Ankle Instability in Different Age Groups: Evaluation of Clinical Outcome Measures. JOIO 55 (Suppl 1), 199–208 (2021). https://doi.org/10.1007/s43465-020-00192-6
[xi] Duzgun, I., Turhan, E. (2018). Proprioception After Shoulder Injury, Surgery, and Rehabilitation. In: Kaya, D., Yosmaoglu, B., Doral, M. (eds) Proprioception in Orthopaedics, Sports Medicine and Rehabilitation. Springer, Cham. https://doi.org/10.1007/978-3-319-66640-2_4
[xii] https://www.collegesportsscholarships.com/balance-training-athletes
[xiii] Yılmaz, O., Soylu, Y., Erkmen, N. et al. Effects of proprioceptive training on sports performance: a systematic review. BMC Sports Sci Med Rehabil 16, 149 (2024). https://doi.org/10.1186/s13102-024-00936-z
[xiv] https://www.psychiatrictimes.com/view/neuroplasticity-after-brain-injury-principles-and-methods-for-postinjury-improvement
[xv] https://neurosciencenews.com/exercise-brain-muscle-26045/
[xvi] Winter L, Huang Q, Sertic JVL, Konczak J. The Effectiveness of Proprioceptive Training for Improving Motor Performance and Motor Dysfunction: A Systematic Review. Front Rehabil Sci. 2022 Apr 8;3:830166. doi: 10.3389/fresc.2022.830166. PMID: 36188962; PMCID: PMC9397687.
[xvii] Ghaderi, M., Letafatkar, A., Thomas, A.C. et al. Effects of a neuromuscular training program using external focus attention cues in male athletes with anterior cruciate ligament reconstruction: a randomized clinical trial. BMC Sports Sci Med Rehabil 13, 49 (2021). https://doi.org/10.1186/s13102-021-00275-3
[xviii] Winter L, Huang Q, Sertic JVL, Konczak J. The Effectiveness of Proprioceptive Training for Improving Motor Performance and Motor Dysfunction: A Systematic Review. Front Rehabil Sci. 2022 Apr 8;3:830166. doi: 10.3389/fresc.2022.830166. PMID: 36188962; PMCID: PMC9397687
[xix] Laumonier T, Menetrey J. Muscle injuries and strategies for improving their repair. J Exp Orthop. 2016 Dec;3(1):15. doi: 10.1186/s40634-016-0051-7. Epub 2016 Jul 22. PMID: 27447481; PMCID: PMC4958098.
[xx] Vincent HK, Brownstein M, Vincent KR. Injury Prevention, Safe Training Techniques, Rehabilitation, and Return to Sport in Trail Runners. Arthrosc Sports Med Rehabil. 2022 Jan 28;4(1):e151-e162. doi: 10.1016/j.asmr.2021.09.032. PMID: 35141547; PMCID: PMC8811510.
[xxi] Rynecki ND, Siracuse BL, Ippolito JA, Beebe KS. Injuries sustained during high intensity interval training: are modern fitness trends contributing to increased injury rates? J Sports Med Phys Fitness 2019;59:1206-12. DOI: 10.23736/S0022-4707.19.09407-6
[xxii] Yılmaz, O., Soylu, Y., Erkmen, N. et al. Effects of proprioceptive training on sports performance: a systematic review. BMC Sports Sci Med Rehabil 16, 149 (2024). https://doi.org/10.1186/s13102-024-00936-z
[xxiii] Kattan AE, AlHemsi HB, AlKhawashki AM, AlFadel FB, Almoosa SM, Mokhtar AM 2nd, Alasmari BA. Patient Compliance With Physical Therapy Following Orthopedic Surgery and Its Outcomes. Cureus. 2023 Apr 6;15(4):e37217. doi: 10.7759/cureus.37217. PMID: 37159781; PMCID: PMC10163936.
[xxiv] Kattan AE, AlHemsi HB, AlKhawashki AM, AlFadel FB, Almoosa SM, Mokhtar AM 2nd, Alasmari BA. Patient Compliance With Physical Therapy Following Orthopedic Surgery and Its Outcomes. Cureus. 2023 Apr 6;15(4):e37217. doi: 10.7759/cureus.37217. PMID: 37159781; PMCID: PMC10163936.
